What is Gut Health?
Although Hippocrates hypothesized that all diseases begin in the gut over 2,000 years ago, research is recently beginning to truly understand the massive impact that gut health has on overall health, wellbeing and disease control.
The truth is, the gut and its functions are extremely complex. The human body is composed of equal if not more bacteria than cells. We are basically bacteria-bipeds wandering this planet. Only about 10% of our cells are truly human, while the majority is microbial.
We are in an age when transplanting fecal matter (poop) from one person into another is a “thing.” An extremely effective “thing” curing over 90% of patients with Clostridium difficile. But nonetheless, that’s how damaged human’s microbial systems have become.
Better questions we can now answer: How did this happen? And how do we fix it?
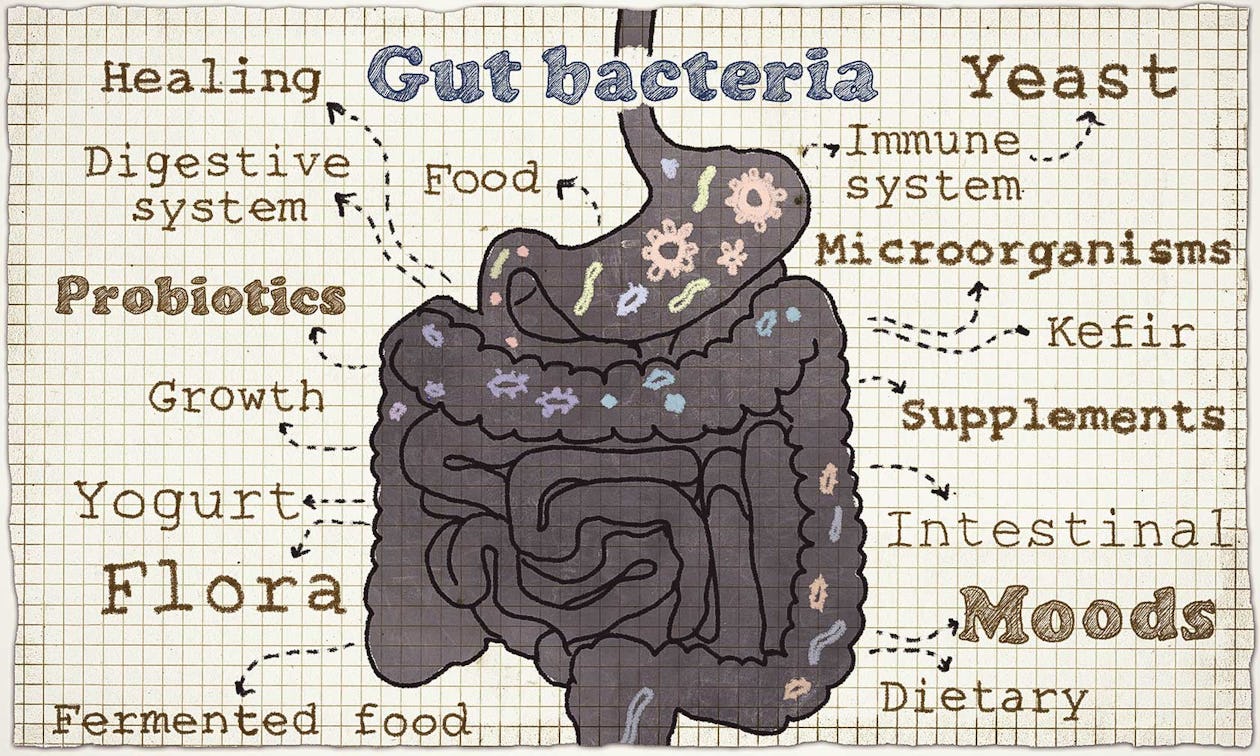
The human body is one ecosystem with trillions of micro-organism inhabitants. This is called the human microbiome. We could not live without this massive colony of bacteria. They are in our eyes, skin, digestive and respiratory system.
The largest colony of microbes reside in our digestive system. There’s an entire world going on in there, with certain species performing different functions. Without gut flora, humans would not be able to survive.
Gut flora can be categorized into three groups:
â Beneficial (essential) flora: These are the most important and most abundant microbes (bacteria) found in a healthy individual. Key beneficial players: Bifidobacteria, Lactobacteria, Propionobacteria, E. Coli (physiological strains only), Peptostreptoccocci and Enterococci.
â Opportunistic flora: These microbes have various functions in different combinations. In a healthy body, opportunistic flora is tightly controlled and regulated by the beneficial bacteria. However, in a compromised immune system, these guys can stray and cause health problems. Key opportunistic players: Bacteroids, Peptococci, Staphylococci, Streptococci, Bacilli, Clostridia, Yeasts, Enterobacteria, Fuzobacteria, Eubacteria, Catenobacteria, etc.
â Transitional flora: These microbes are consumed on a daily basis through the environmental toxins and processed food. As long the gut is protected by beneficial bacteria, these microbes will pass through our digestive system without harm. But if it’s damaged, transitional flora can lead to disease. Key transitional players: toxins, chemicals, parasites, bacteria in undigested food and drink.
Immune System & Gut Health

Approximately 80% of our immune system is located in the gut. Basically if your beneficial microbes are M.I.A., there’s a good chance you’re getting sick, my friend. The Mucosal Barrier of the Gastrointestinal (GI) tract is built to allow very small fully digested particles through.
However, when the GI tract becomes stressed, the tight junctions between the cells lining of our GI tract or enterocytes become loose. This allows the unchecked entry of bigger particles into the bloodstream. Your body then sees these larger particles as foreign and activates the immune system just like it would for any pathogen.
The problem is that your immune system has a great memory (via memory B cells). They don’t care what exactly that large particle is. To your immune system, it’s just an intruder that needs to be pulverized. Thus, if you have intestinal permeability depending on what larger particles get through, your immune system can start attacking literally any items that you commonly eat like tomatoes, garlic, cucumbers, even a lean piece of grass-fed steak.
The problem doesn’t end there because if a large particle gets through that looks similar to thyroid, ovarian, adrenal, or mucosal tissue, you may have just set the stage for an auto-immune disease – your own immune system now sees yourself as foreign. This is called molecular mimicry and this chain of events is not something to take lightly.
Energy Metabolism
Without a well-balanced gut flora, digestion and absorption cannot be optimal. This bacteria has the ability to break down protein, carbohydrates, fat and fiber. “By-products of bacterial activity in the gut are very important in transporting minerals, vitamins, water, gases and many other nutrients through the gut wall into the bloodstream.”
Take Away: Even if you followed a ’perfect’ diet consuming all the “superfoods” in the world, you cannot combat a damaged gut flora. It’s essential to heal the gut first. Then you will be able to able to efficiently digest and absorb healthy foods and supplements. Fiber and lactose (milk sugar) are two substances that require good bacteria for digestion.
Most people don’t produce lactase–the enzyme that breaks down lactose–after infancy. But why then can some people handle dairy while others cannot? This is because these individuals have a lot of lactose-digesting bacteria; one of the most notable ones being E. Coli. Yes, this is same bacteria that also can make us sick.
However, if your gut is populated by physiological strains of E. Coli, you are better equipped to fight off the pathogenic (bad) species of E. Coli.
What Compromises the Microbiome?
The integrity of the gut flora has its roots far before your parents conceived you. Did dad follow a strict Ramen-noodle diet in college? Was mom hanging out with Ben & Jerry on the reg while you were in her tummy? Not to put the blame on our folks’ diet, but it is one contributing factor to a baby’s microbiome among many other factors, including:
Birth & Infancy
â C-section babies
â Bottle-fed babies
Antibiotics
â Penicillins
â Tetracyclines
â Aminoglycosides
â Antifungal antibiotics
â Antibiotics wipe out all bacteria–the bad and the good. So, although necessary at times, a dose of these drugs will inherently leave you immune-compromised.
Other Drugs
â Pain killers
â Steroids
â Contraceptives
â Sleeping pills
â Heartburn medication
Processed Foods
â Sugar & processed carbohydrates
â Grain fiber
â Food sensitivities – common allergens and food sensitivities wreak havoc on your digestive system eventually leading to GI tract shutdown, a blunted brush border, dysbiosis, and poor gut health.
Disease
â Infectious disease
â Viral infections
â Chronic illness
â Alcoholism
â Dysbiosis – or inappropriate ratio of good vs. bad bacteria residing in the gut. This is the topic of entire books and articles, but in the simplest terms: you are the wolf that you feed. Healthy bacteria thrive on colorful fruits and vegetables, bad bacteria thrive on sugar, artificial sweeteners, and unhealthy fats. Also, if you have transit time issues, it is very likely that you have some kind of dysbiosis and brain to gut axis issue.
Stress
â Short-term stress (recovers fairly easy)
â Prolonged stress (permanent damage)
Other Factors
â Old age
â Over physical exertion
â Surgery
â Pollution
â Toxic substance exposure/ingestion
â Extreme climates
â Environmental Toxins – items like BPA, BT Toxin (found in GMO corn), and Glyphosate (AKA Round-Up).
â Intestinal parasites, microbial infestations, or fungal overgrowth – this is much more common than you might think. 80-90% of our population is believed to have some kind of unwanted GI intruder.
Take away: Think twice before taking antibiotics and popping any over-the-counter or prescribed medication. Please, do not take this fundamentally. Just don’t go running to the doctor the second you have the sniffles. Sure, a Z-Pack will probably make you feel better in the short term, but you’re wiping out all of the good bacteria along with the bad. Plus, overuse of antibiotics leads to antibiotic resistance. So when you really need those meds to work, they may not.
Avoid processed food. It sounds simple, but it’s not with over 80% of the American food supply being altered or processed in some way.
Control “extreme” behaviors. This can be any obsessive act or habit from partying too much to over-exercising to everything in between. Too much of a bad OR good thing causes stress to the body and damages the gut flora.
Practice TLC in the most natural environment possible. You probably won’t witness the lasting effects of recycling that glass bottle but your body will. By removing yourself from life’s stressors aka your 8×8 work cubicle and entering a local park surrounded by lots of green, you will inherently avoid many of those damaging factors.
How to Establish a Healthy Gut?

The information on how to help fix gut health could fill an entire book, let alone an article. While we obviously can’t go into that kind of detail here, we can give you some simple fixes that will get you started on the right track.
Restore Stomach Acid Production
The first step in restoring stomach acid production is addressing any factors that are inhibiting it. This means getting tested for H. pylori if you suspect it, taking steps to manage chronic stress and avoiding acid-suppressing drugs.
The next step is to take hydrochloric acid (HCL). Taking HCL can often help kick start the body’s own acid production. HCL helps limit digestive problems as well as the potentially serious consequences of low stomach acid (such as decreased nutrient absorption, bacterial overgrowth, and increased susceptibility to infection.
Be aware that HCL should always be taken with pepsin — or, better yet, acid-stable protease — because it is likely that if the stomach is not producing enough HCL, it is also not producing enough protein digesting enzymes.
Replace Digestive Enzymes
As mentioned above, the single most important step in increasing digestive enzyme production is by restoring stomach acid production.
This will give the chyme entering the small intestine the proper pH level (acidity), which is what stimulates the pancreas to produce enzymes. Managing chronic stress and ensuring adequate micronutrient (co- enzyme) intake are also important.
Diet
This one is a little harder to give a quick overview of, because there are so many potential causes, and some of those causes require a fairly complex approach. What we can do is give you a few general tips that are helpful in most circumstances, regardless of the cause.
The first step would be to cut out gluten. Gluten leads to increased intestinal permeability if you have a gluten allergy/sensitivity or not (via activation of the zonulin pathway). Gluten is not your friend.
Also, just two alcholic beverages will cause damage to the intestinal lining and in turn intestinal permeability. A night of bottle service and pizza is a fantastic way to ramp yourself for an incredible inflammatory response and maybe even good ol’ autoimmune disease.
None of this sounds sexy or fun. Sorry, but we don’t make the rules and we’ve found a fair number of people who are weight loss resistant in our practice.
These people try everything but can’t lose body fat and constantly crave sugar. This is because whenever your immune system is running wild, you will be in a perpetual state of sugar burning and have zero shot at burning stored fat no matter how little you eat or how much you exercise.
Fixing the GI tract and securing up the junctions between our enterocytes is the first step on the road to putting out the inflammatory fire and having a real opportunity to incinerate visceral fat or the bulge around the middle.
The next step would be trying some tweaks to your existing Paleo or “real food” diet. (You are on a Paleo or “real food” diet, aren’t you? If not, that is the first step. Here are three diet fixes we’ve found to be helpful, and they’re listed in the order we suggest you try them:
â Add Fermented Food. Raw, fermented foods like sauerkraut, kimchi, kefir or beet kvass are rich in enzymes and should be consumed regularly if tolerated.
â Try an Elimination diet. Cut out all gluten, dairy, and sugar for a minimum of two weeks (6 weeks is ideal). Begin to add one food back into your diet. A piece of sprouted, whole-grain bread is a good start. Now you begin the waiting game.
â GAPS diet. The GAPS diet is a comprehensive, anti-inflammatory, gut-healing diet. It’s especially helpful with SIBO, dysbiosis, and inflammatory bowel disease (IBD).

Along with these diet tips, we suggest you start adding these probiotic strains and supplements to you daily protocol. Supplemental nutrients can be helpful for immediate relief. These include:
â Ox bile. While not technically an enzyme, ox bile is one of the most effective supplements for improving fat absorption.
â Acid stable protease. Improves protein digestion; acid-stable protease is able to survive the low pH of gastric juices to further aid in protein assimilation.
â Pancreatin. A mixture of enzymes produced by the pancreas, including lipase (fat digesting), protease (protein digesting) and amylase (carbohydrate digesting).
â Bromelain. An enzyme found in pineapple that helps with protein digestion, and may have systemic anti-inflammatory effects.
â Ginger. A time-tested digestive remedy. As with HCL, in most cases you will only need to take these nutrients temporarily, until you are able to address the underlying issues. But they can be incredibly helpful in the meantime.
Probiotic Bacteria
More and more research has shown the effectiveness of daily probiotic supplementation on energy metabolism, immune system strength and disease control. Probiotics are strains of beneficial bacteria. Of course, there are thousands of strains of probiotics, so it’s virtually impossible to get every single strain through one probiotic supplement, but there are some heavy hitters that are widely available and crucial to take on a daily basis.
â Lactobacillus acidophilus
â Lactobacillus plantarum
â Lactobacillus rhamnosus
â Bifidobacterium infantis
â Bifidobacterium lactis
Probiotic Yeast
â Saccharomyces Boulardii
Prebiotic
â Organic Jerusalem Artichoke (root)
â Organic Dandelion (leaf)
Digestive Enzymes
â Amylase
â Protease
â Lipase
â Cellulase
â Alpha Galactosidase
â Maltase
â Lactase
â Glucoamylase
â Pectinase
â Xylanase
â Beta Glucanase
â Invertase
â Hemicellulase
â Serratiopeptidase
â Pepsin
Bitter Herbs
Another way to stimulate acid production in the stomach is by taking bitter herbs. “Bitters” have been used in traditional cultures for thousands of years to stimulate and improve digestion. More recently, studies have confirmed the ability of bitters to increase the flow of digestive juices, including HCL, bile, pepsin, gastrin and pancreatic enzymes. The following is a list of bitter herbs commonly used in Western and Chinese herbology:
â Dandelion
â Fennel
â Gentian root
â Ginger
â Beet root
â Goldenseal root
â Milk thistle
â Peppermint
â Wormwood
â Yellow dock
Hydrochloric Acid
â Betaine Hydrochloride
References
1. Mutzel, Mike. Belly Fat Effect: The Real Secret about How Your Diet, Intestinal Health, and Gut Bacteria Help You Burn Fat. Print
2. Arrieta, M. C. “Alterations in Intestinal Permeability.” Gut 55.10 (2006): 1512-520.
3. Kharrazian, Datis. Why Do I Still Have Thyroid Symptoms? When My Lab Tests Are Normal: A Revolutionary Breakthrough in Understanding Hashimoto’s Disease and Hypothyroidism. Garden City, NY: Morgan James, 2010. Print.
4. Davis, Reed. “Functional Diagnostic Nutrition – Lecture Series 4.” FDN Certification. 8 Aug. 2015.


)